
 Last year, I wrote a LinkedIn Article titled “To be or not to be: Just because you CAN, doesn’t mean you SHOULD.” The point was straightforward. Passion and good science are not enough. They never really were. That post was a reaction to what I was seeing across early-stage biotech and MedTech at the time. The environment has not eased since then. If anything, the bar has moved higher.
Last year, I wrote a LinkedIn Article titled “To be or not to be: Just because you CAN, doesn’t mean you SHOULD.” The point was straightforward. Passion and good science are not enough. They never really were. That post was a reaction to what I was seeing across early-stage biotech and MedTech at the time. The environment has not eased since then. If anything, the bar has moved higher.
The requirements for viability are more stringent today than they were even a year ago. Early-stage capital remains difficult to access, particularly at the seed and Series A stages, unless a company has human proof of concept. Angel investors want de-risking. Most venture funds will not underwrite the earliest technical risk. Government funding used to fill that gap. The uncertainty around the reauthorization of innovation investment programs has made it harder to hit commercially meaningful milestones at exactly the stage when companies need that support most. Until policy catches up, founders are forced to seek private capital that is increasingly selective and unforgiving.
This shifts the question founders need to ask themselves. It is no longer whether an idea is interesting or even whether it addresses an unmet need. The question is whether the idea can survive the current validation threshold. That threshold is no longer defined by enthusiasm or momentum. It is defined by evidence, timing, and a clear path to value creation that stands up to scrutiny.
Commercial realism remains the most common failure point. Founders and CEOs are almost always optimistic about their opportunity, and they should be. If the CEO is not the champion, no one else will be. The problem arises when optimism replaces rigor. Market size is often overstated. Competitive dynamics are underestimated. Pricing and reimbursement assumptions are built on hope rather than data. Real market assessments require primary customer discovery paired with precedent sales data, both top-down and bottom-up. They also require discipline about who the customer is and where adoption will realistically occur.
Differentiation has also changed. Incremental improvements used to matter. Slight changes in dosing or convenience could be enough in some cases, but that still holds only if the market signals that it values those changes. In many therapeutic and digital health categories, that bar has risen. The existence of a standard of care, even an imperfect one, changes everything. Workarounds that are cheaper and good enough are formidable competitors. A fourth- or fifth-line product rarely succeeds just because the total addressable market is significant. Investors are not persuaded by big numbers without a sophisticated explanation of what portion of that market is reachable and why.
Health economics can no longer be an afterthought. Payers are not focused on novelty. They are focused on sustainability. Cost effectiveness, total cost of care, and system-level impact matter early, not late. Clinical development strategies that ignore this reality tend to produce assets that struggle to gain traction even if they reach approval.
Manufacturing and supply chain considerations are now decisive factors in viability. Fully burdened cost modeling should be mandatory, not optional. Many promising concepts fail when exposed to the realities of sourcing, scale-up, tech transfer, and CDMO capacity. Lead times for specialized reagents, limited suppliers, geopolitical pressures, and competition from larger customers all introduce risks that can derail timelines and margins. Profitability estimates that are not grounded in real quotes and realistic assumptions are unreliable. A product that cannot be manufactured profitably at scale is not a product. It is an experiment.
Intellectual property expectations have also hardened. Venture investors continue to favor novel chemical entities with enforceable composition-of-matter claims. Method-of-use claims and simple repurposing strategies remain difficult to defend commercially. Off-label use, generic substitution, and payer resistance erode value quickly. Repurposing can be both capital and clinically efficient, but unless there is a credible way to lock the market through delivery technology, owned chemistry, or a pricing model that holds, it is rarely attractive to institutional capital. The irony is that some of the most efficient paths to patient benefit struggle the most under current investment models.
Clinical adoption risk extends far beyond efficacy. I look at alternatives already in use and ask who they fail and why. I look at early predictors of response and whether patient selection is feasible. I look at whose pain point is being addressed and whether that aligns across providers, patients, payers, and regulators. Evidence requirements vary by stakeholder, and the costs and time required to satisfy them must be modeled honestly. I also look closely at who makes the buying decision and how the product would be sold. Adoption fails as often for psychological and behavioral reasons as it does for scientific ones.
Deciding whether to move forward, pause, or walk away requires discipline. Founders need to evaluate unmet need, solution fit, market opportunity, IP defensibility, validation requirements, development and manufacturing plans, regulatory and reimbursement pathways, financial models, and exit logic together. Weaknesses in any one area can undermine the entire effort. The willingness to stop is not a sign of failure. It is a sign of judgment. In this environment, the threshold for validation is higher across the board, even in areas that remain attractive to pharma and investors.
This is where an experienced, external perspective matters. A short, focused conversation can surface gaps that would otherwise take years and significant capital to discover. Stress-testing assumptions early saves time, money, and energy. Not every idea should become a company. Not every asset belongs in a pipeline. The goal is not to build something at all costs. The goal is to build something that has a real chance of reaching patients and creating value along the way.
Being in the business of innovation means living with uncertainty and learning constantly. It also means making hard calls sooner rather than later. Just because you can still does not mean you should. The difference between the two has never mattered more.
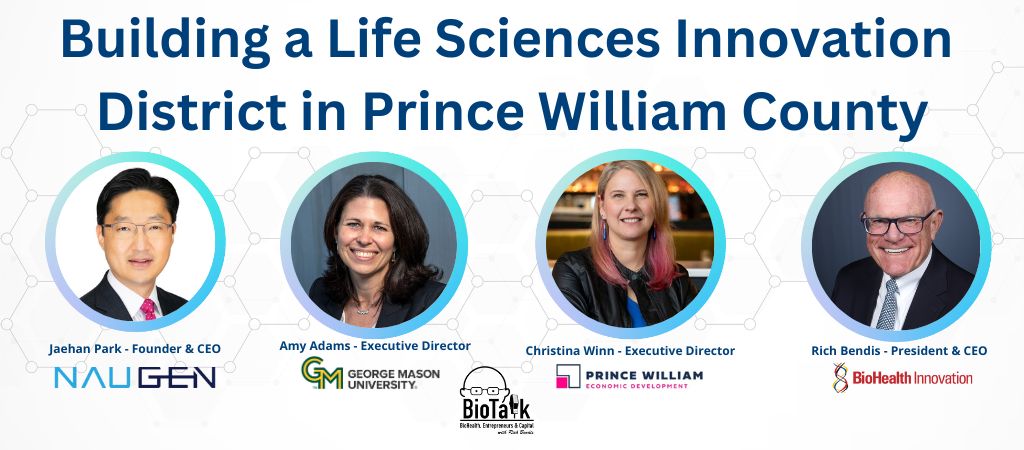
 This episode of the BioTalk with Rich Bendis Podcast brings together leaders from industry, academia, and economic development to unpack the vision behind a new life sciences Innovation District anchored in Prince William County. With introductions to NAUGEN, George Mason University’s Institute for Biohealth Innovation, and the Prince William County Department of Economic Development, setting the stage for how each organization contributes to the district’s foundation. The guests discuss the life science assets, research strengths, and translational capabilities that define the district and explain why it is well-positioned to support biotechnology and advanced R&D companies.
This episode of the BioTalk with Rich Bendis Podcast brings together leaders from industry, academia, and economic development to unpack the vision behind a new life sciences Innovation District anchored in Prince William County. With introductions to NAUGEN, George Mason University’s Institute for Biohealth Innovation, and the Prince William County Department of Economic Development, setting the stage for how each organization contributes to the district’s foundation. The guests discuss the life science assets, research strengths, and translational capabilities that define the district and explain why it is well-positioned to support biotechnology and advanced R&D companies.
The podcast explores how the partnership between Prince William County, George Mason University, and the City of Manassas came together, outlining the distinct roles each plays in advancing a shared strategy. The episode also introduces the NISA program, detailing how it supports companies seeking a soft-landing pathway into the district, the types of organizations best suited for the program, and the facilities, talent, and collaborative resources participants can access both immediately and over time.
Listen now via your favorite podcast platform:
Apple: https://apple.co/4p94Dqe
Spotify: https://bit.ly/3Y7dJZw
iHeart Podcasts: https://ihr.fm/3KLV7v4
Amazon Music Podcasts: https://amzn.to/4pajS1P
YouTube Music Podcasts: https://bit.ly/4phRV8I
TuneIn: https://bit.ly/44GoG7Y
Editing and post-production work for this episode was provided by The Podcast Consultant (https://thepodcastconsultant.com).
Jaehan Park is Founder and CEO of NAUGEN, a global innovation accelerator advancing novel technologies across life sciences and deep tech. With more than 25 years of experience in strategy and business development, he has led collaborations spanning cancer immunotherapy, vaccines, and biologics with global pharmaceutical companies and academic institutions. He leads the NISA Program in partnership with George Mason University and serves as a Mentor-in-Residence at KIC DC, supporting international startups entering U.S. markets.
Amy Adams is Executive Director of George Mason University’s Institute for Biohealth Innovation, where she advances biohealth research and innovation across more than 300 faculty and thousands of students. Her work focuses on partnerships, shared research infrastructure, and building hubs that connect academia with industry. She is co-leading the development of the Innovation District anchored at Mason’s SciTech campus and serves on the boards of BioHealth Innovation and the Association of University Research Parks.
Christina Winn leads the Prince William County Department of Economic Development, guiding investment, business growth, and redevelopment efforts across one of Virginia’s largest counties. She is overseeing the development of a research-driven Innovation District in partnership with George Mason University and the City of Manassas, supported by a GO Virginia grant. Her career includes leading large-scale economic development initiatives that have driven significant capital investment, job creation, and national visibility for the region.

 BioHealth Innovation is expanding its Entrepreneurs in Residence (EIR) network and is seeking experienced leaders at the intersection of biohealth and advanced technologies, including artificial intelligence and quantum computing.
BioHealth Innovation is expanding its Entrepreneurs in Residence (EIR) network and is seeking experienced leaders at the intersection of biohealth and advanced technologies, including artificial intelligence and quantum computing.
This call is for seasoned operators with a strong commercialization background. Ideal candidates have taken innovations from concept through market entry, licensing, spinout, or acquisition, and understand the realities of regulatory pathways, customer discovery, fundraising, and scale. Experience working with startups, academic technologies, government labs, or early-stage venture-backed companies is essential. EIRs serve in a part time advisory role with BHI, working flexibly alongside other professional commitments while contributing hands on commercialization expertise.
We are particularly interested in EIRs who can translate AI and quantum capabilities into practical biohealth applications, including drug discovery, diagnostics, clinical research, manufacturing, data analytics, and health system innovation. The role requires comfort working across technical, business, and stakeholder environments.
EIRs work closely with entrepreneurs, researchers, and partners across the BioHealth Capital Region and nationally. Engagements may include advising project teams, supporting partner initiatives, guiding commercialization strategy, and mentoring founders navigating early growth decisions.
This is an opportunity to contribute deep expertise to high-potential biohealth innovations while remaining connected to a collaborative, mission-driven ecosystem.
Interested candidates should contact BHI Founder, President, and CEO, Rich Bendis at rbendis@biohealthinnovation.org, with a summary of their background, commercialization experience, and areas of technical focus.

 by Jonathan Kay, MPP, Managing Partner, Health Market Experts & BioHealth Innovation, Inc. Entrepreneur-in-Residence
by Jonathan Kay, MPP, Managing Partner, Health Market Experts & BioHealth Innovation, Inc. Entrepreneur-in-Residence
Healthcare is complicated. Communicating effectively doesn’t need to be.
For a new medical technology, biologic, pharmaceutical, or digital health solution, a critical element of go-to-market strategy (GTM) and initial commercial success is messaging.
But messaging often doesn’t get the attention it deserves.
GTM messaging could include messages to any: physicians, hospital administrators, policy makers, patients, caregivers, payers, and more.
This post kicks off our 7-part series on Optimizing Launch Messaging 🚀, where we will share 7 valuable tactics to help achieve your goals related to access, commercial success, and improved patient outcomes.
Tactic 1: Test, Don’t Guess
The first step to optimizing launch strategy is embracing a data-driven mindset:
Healthcare markets are complex in so many ways. Think of the scientific, clinical, regulatory, reimbursement, and competitive landscape. Testing in a complex and changing environment helps minimize risk and maximize potential.
Companies run clinical trials to test the impact of a therapy. Similarly, commercial teams should test their launch communications to ensure they are effective and safe. That is, are the messages clear, credible, and persuasive? Do the messages avoid unintended consequences?
Why test messages? We test messages to:
- Understand unmet needs
- Assess competitive differentiators
- Understand which messages resonate and why
- Learn how to motivate appropriate behavior
Do you have a positive example from when you tested messages in advance of using them? Share your thoughts below!
At Health Market Experts, we make corporate and brand messaging more efficient and effective. If your organization is preparing to launch a product or a campaign, connect with us to learn more about how we can help you develop and execute your launch plan and maximize success. Ask us about message awareness and attribution, too.
This post was written with NI not AI (written by a human using natural intelligence).
This post expands on content I previously wrote as a blog at Catalant and delivered in guest lectures at Rutgers Business School.
Visit https://www.linkedin.com/in/jonathan-kay-healthcare/ to connect with Jon on LinkedIn.
